Peak flu season doesn’t just strain clinical staff, it stress-tests every piece of healthcare IT infrastructure that keeps patient flow moving. During flu season surges, even minor IT failures can cascade into delayed check-ins, longer wait times, overwhelmed staff, and disrupted care delivery, especially when on-site support isn’t immediately available.
For healthcare operations leaders, COOs, and service delivery managers, the stakes are high. Proactive healthcare IT support, paired with truly nationwide field services and an AI-human hybrid help desk, helps healthcare organizations maintain uptime, protect patient experience, and support frontline teams during their most demanding months.
This guide explores why traditional support models strain during surges and how a proactive, managed approach can keep your facilities running smoothly when it matters most.
Why Flu Season Exposes Weak Healthcare IT Support Models
The influx of patients during respiratory virus season creates a perfect storm for IT infrastructure. It is not just about more people in the waiting room, it is about the velocity of digital transactions required to treat them.
Seasonal Surge in Volume and Strain
Flu season typically spans October through March, a window where patient volumes can surge dramatically. CDC data often shows positivity rates jumping significantly within months, driving a corresponding increase in patient visits. Every additional patient represents a sequence of digital interactions: a check-in at a kiosk, a verification at a registration desk, a vital signs entry on a workstation, and a prescription transmission.
This increased utilization strains hardware and networks.
- Patient check-in kiosks face intense physical wear, leading to degraded touchscreens or jammed thermal printers.
- Point-of-care workstations experience battery failures and connectivity issues from constant movement and use.
- Telehealth usage often spikes as patients seek remote care, stressing bandwidth and cart peripherals.
- Wireless access points can go down at any time. This takes all technology offline and can prevent patients from getting the information they need.
The Failure of Reactive Support
Reactive IT support, often using a break/fix model, is not capable of handling the pressure of healthcare demands. When a vital system crashes during a peak period, the sole critical measure of success becomes the time it takes for a technician to be dispatched, known as the truck roll.
In a reactive model, a downed kiosk forces patients to the front desk, creating bottlenecks that ripple through the entire appointment schedule. If a nurse’s workstation fails, clinical documentation slows, and login friction can cost clinicians cumulative hours per shift. During high-demand periods, these delays are not just inconveniences; they are operational liabilities that degrade patient throughput and increase the risk of infection spread in crowded waiting areas.

What “Nationwide Healthcare IT Support” Really Means
Many providers claim nationwide coverage, but for healthcare leadership, understanding the structural nuances behind this term is essential. The method of service delivery directly influences accountability, security, and response speeds, especially during a crisis.
Claimed Coverage vs. Operational Reality
In the domain of IT field services, “nationwide” is often a marketing holistic that obscures significant variations in capability. The industry is divided into two primary operational models: self-performing entities and service aggregators.
- Aggregator Model: A significant portion of the market operates on an aggregator model. The entity holding the contract does not directly employ the technicians. Instead, they act as a central dispatch node, leveraging a network of independent contractors or “gig economy” workers. While this allows for broad theoretical footprints, it introduces variability in training, equipment, and accountability.
- Self-Performing Model: Self-performing organizations employ their own Field Service Technicians (FSTs) or maintain direct control over a vetted partner network. This model typically yields higher consistency in service delivery, as the provider manages the fleet, tooling, and professional development of the staff.
The Importance of Accountability
Healthcare environments require higher accountability than retail or general office settings. The chain of custody regarding site access, data handling, and asset management must remain unbroken. A self-performing or tightly managed model offers tighter control over compliance requirements, such as HIPAA training and immunization verification, because the provider has direct HR authority over the staff entering the facility.
The Operational Risk of Rural and Distributed Healthcare Locations
The disparity between urban and rural healthcare IT support reflects the broader infrastructure divide. For healthcare COOs managing networks that include rural clinics, critical access hospitals, or home health operations, this divide represents a significant operational risk.
The Breaking Point: Rural Locations
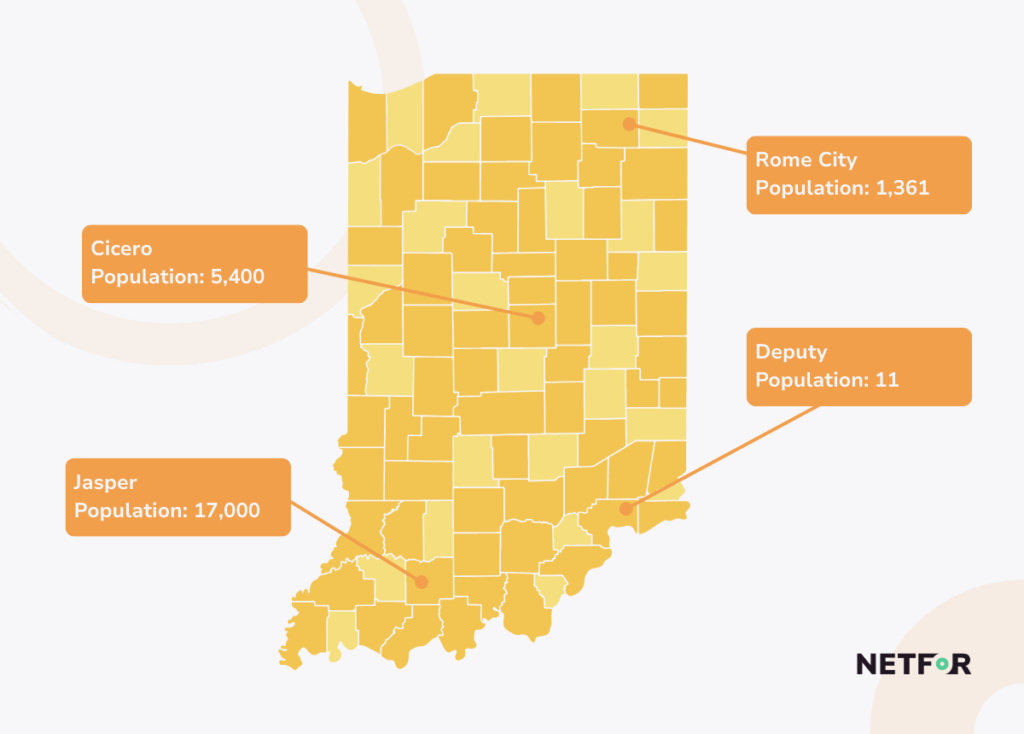
Rural locations are often the breaking point for healthcare IT support. Operational data confirms a stark contrast in response capabilities. Just as rural EMS response times are longer than national averages, IT field service response times in rural areas suffer from a scarcity of qualified technical labor.
The distance required for a technician to travel to a rural site increases the Mean Time To Repair (MTTR) substantially. In many cases, a standard SLA in an urban center becomes a “best effort” SLA in a rural location due to the logistical complexity of dispatch.
Infrastructure Fragility
Rural healthcare facilities often operate with older infrastructure and less redundancy, making them more vulnerable to outages. Legacy hardware may struggle with modern software demands, and broadband reliability can complicate remote diagnosis.
Consider a clinic relying on a long-drive technician strategy. If a critical router fails, the clinic might be unable to process patients for days while waiting for a technician to travel from the nearest metropolis. This results in fewer patients seen, lost revenue, and a community left without access to care during a critical health season.
Mitigating the Risk
To counter these risks, healthcare organizations must vet providers on their specific rural capabilities. Advanced providers use geofencing and dynamic planning to optimize routes. For rural locations, the most effective strategy is often to bypass the repair attempt entirely. Providers that can stage inventory at regional depots can ship a pre-configured replacement overnight, a swap-out model that is often faster and more reliable than waiting for a technician to diagnose and repair a complex hardware failure on-site.
How Field Services, Help Desk, and AI Work Together to Reduce Downtime
The most efficient IT support model is one that resolves issues before a technician is ever dispatched. Leading healthcare IT strategies integrate remote Help Desk capabilities with Field Service dispatch in a unified workflow. This model leverages technology to optimize human labor and reduce downtime.
AI-Human Hybrid Help Desk Triage
High-performing organizations attempt to resolve issues at the lowest cost level (Tier 1) before escalating to the highest cost level (Field Service/Truck Roll).
An AI-human hybrid help desk is central to this strategy. AI-powered chatbots and virtual assistants can handle routine queries and simple troubleshooting, freeing up human agents to handle complex clinical issues. This reduces ticket backlogs and call wait times, ensuring that a nurse needing urgent password assistance isn’t stuck on hold.
Reducing Unnecessary Truck Rolls
Effective triage ensures that field technicians are reserved for true hardware failures or physical layer issues. Remote teams can often diagnose the specific part needed before a dispatch occurs. For example, a remote agent might identify a failing power supply on a kiosk. By diagnosing this upfront, the technician arrives with the correct part in hand.
This diagnostic accuracy directly improves the First Run Rate (FRR), a critical KPI. If a technician arrives but lacks the skills or parts to fix the issue, a second visit is required, extending downtime exponentially. Netfor, for instance, maintains a First Run Rate (FRR) of 95% and a First Call Resolution Rate (FCR) of 92%, metrics that demonstrate the power of accurate triage and preparation.
Smart Hands Support
In scenarios where a full-time senior engineer is not required on-site, providers like Netfor can staff Smart Hands services. A qualified field technician acts as the eyes and hands for a high-level remote engineer. Using video links or augmented reality tools, a remote Network Architect can guide a local technician through a complex configuration. This allows rural locations to access high-level expertise without the cost and delay of flying in a senior engineer, bridging the gap between local availability and centralized expertise.
What Healthcare Leaders Should Look for in Managed IT Support Services
When evaluating a managed IT support partner, healthcare leaders must look beyond basic technical capabilities. The “who” is as critical as the “what” in healthcare field services.
Vetting, Compliance, and Credentialing
Healthcare facilities are controlled environments. The introduction of third-party technicians introduces security, privacy, and health risks. Therefore, the vetting protocols of a field service provider are paramount.
- Joint Commission & HIPAA: Contractors must provide certification of competency. Facilities must be able to prove to auditors that the technician touching a clinical device was qualified to do so. Technicians must also undergo HIPAA training to understand the privacy implications of working around Protected Health Information (PHI).
- Immunization Requirements: During flu season, the lack of a current flu shot can bar a technician from entry. Providers must track and enforce health requirements, including TB testing and Hep B vaccinations.
- Background Checks: Security vetting should distinguish between “gig economy” aggregators and professional managed service providers. Standard vetting typically involves a 7-year criminal background check, but high-security environments often require more rigorous screening, including OIG exclusion list checks.
Cost and Scalability Advantages
Maintaining an internal field service team requires carrying high fixed costs that remain static regardless of demand. Outsourcing converts these fixed costs into variable costs; organizations pay for the dispatch only when needed.
This scalability is crucial during surges. An internal team sized for normal volume will be overwhelmed during flu season, leading to backlogs and burnout. A nationwide provider has the depth of bench to scale up resources on demand, absorbing the seasonal spike without the healthcare organization needing to hire temporary staff.
Proven Success: Marathon Health
The value of scalable support is evident in real-world applications. Marathon Health, operating a network of nearly 800 health centers, needed to improve nationwide technology reliability. They partnered with Netfor to establish comprehensive technical support across all locations.
The result was a unified model that delivered local reach with national coverage. By implementing a complete network modernization and establishing rigorous quality standards, Marathon Health saw a significant reduction in technical support tickets and eliminated connectivity disruptions between exam rooms. This allowed their clinicians to move seamlessly during patient visits, proving that the right partner can turn IT from a bottleneck into a strategic asset.
(Read the Case Study Here: Marathon Health Success Story)
Integrated Call Center and Field Services
Similarly, integrated support models that combine call center capabilities with field services provide a holistic view of the patient and clinician experience. By analyzing data from the help desk, organizations can identify recurring issues and deploy field resources proactively, rather than reacting to outages after they occur.
(Source: Healthcare Call Center Capabilities)
Be Ready for Any Season
Flu season turns IT reliability into a care delivery issue. When patient volumes peak and clinical teams are stretched thin, the last thing a healthcare organization needs is a stalled workflow caused by a preventable IT failure.
Nationwide healthcare IT support must be proven, not assumed. It requires a partner who understands the operational realities of rural coverage, the necessity of rigorous compliance, and the critical nature of response times.
By adopting a unified model that combines managed IT support, an AI-human hybrid help desk, and truly nationwide field services, healthcare leaders can reduce downtime, protect patient throughput, and reduce strain on their teams. The ability to fix a broken kiosk in a rural clinic during a flu outbreak in Waterville, Maine, is not just an IT success. It is a patient care victory.

